Overview
Vulvar Cancer
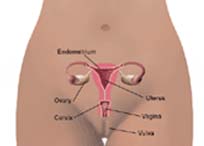
What is the vulva?
The vulva is the external portion of the female genital organs. It includes: -
- labia majora - two large, fleshy lips, or folds of skin
- labia minora - small lips that lie inside the labia majora and surround the openings to the urethra and vagina
- vestibule - space where the vagina opens
- prepuce - a fold of skin formed by the labia minora
- clitoris - a small protrusion sensitive to stimulation
- fourchette - area beneath the vaginal opening where the labia minora meet
- perineum - area between the vagina and the anus
- anus - opening at the end of the anal canal
- urethra - connecting tube to the bladder
What is vulvar cancer?
 Vulvar cancer is a malignancy that can occur on any part of the external organs, but most often affects the labia majora or labia minora. According the American Cancer Society, about 3,490 cases of cancer of the vulva will be diagnosed in the US in 2007. Cancer of the vulva is a rare disease, which accounts for 0.6 percent of all cancers in women, and may form slowly over many years. Nearly 90 percent of vulvar cancers are squamous cell carcinomas. Melanoma is the second most common type of vulvar cancer, usually found in the labia minora or clitoris.
Vulvar cancer is a malignancy that can occur on any part of the external organs, but most often affects the labia majora or labia minora. According the American Cancer Society, about 3,490 cases of cancer of the vulva will be diagnosed in the US in 2007. Cancer of the vulva is a rare disease, which accounts for 0.6 percent of all cancers in women, and may form slowly over many years. Nearly 90 percent of vulvar cancers are squamous cell carcinomas. Melanoma is the second most common type of vulvar cancer, usually found in the labia minora or clitoris. Other types of vulvar cancer include: -
- adenocarcinoma
- Paget's disease
- sarcomas
- verrucous carcinoma
- basal cell carcinoma
How can vulvar cancer be prevented?
The cause of vulvar cancer is not known at this time, however, certain risk factors are suspected as contributors to the development of the disease.
Suggestions for prevention include: -
- Avoid known risk factors when possible.
- Delay onset of sexual activity.
- Use condoms.
- Do not smoke.
- Have regular physical checkups.
- Have routine Pap tests and pelvic examinations.
- Routinely check entire body for irregular growth of moles.
Signs and Symptoms
Vulvar cancer forms in the vulva, the area around the external genital organs on a woman.The vulva includes the following parts: -
- Labia - The lips around the opening of the vagina
- Clitoris - A small mass of tissue at the opening of the vagina
- Bartholin's Glands - The small mucus-producing glands on either side of the vaginal opening
Vulvar cancer is relatively rare, and typically affects Caucasian women over the age of 60, although the condition can occur in younger women and those of all ethnicities.
Other risk factors for the condition include: -
- Smoking
- Taking steroids or other drugs that weaken the immune system
- Genital warts caused by the sexually transmitted human papillomavirus (HPV)
Common symptoms of vulvar cancer may include: -
- Vulvar itching that lasts more than one month
- A cut or sore on the vulva that won't heal
- A lump or mass on the vulva
- Unexplained vulvar pain
- Bleeding from the vulva that is different from your usual monthly bleeding
- Burning in the area that lasts even after your doctor has treated the burning
- Any change in size, color or texture of a birthmark or mole in the vulvar area
Diagnosis
It is important to note that if detected and treated early, vulvar cancer has a high cure rate. Therefore, it is essential that you visit your doctor for a definite diagnosis. In making a diagnosis, your doctor will first review your medical history, ask about any symptoms you are experiencing and conduct a thorough physical exam.The following tests also may be performed: -
- Pelvic Exam - This test involves feeling the uterus, vagina, ovaries, fallopian tubes, bladder and rectum to find any abnormality in their shape or size.
- Ultrasound - This test uses high-frequency sound waves to create images of organs and systems within the body. These waves, which cannot be heard by humans, create a pattern of echoes called a sonogram. Healthy tissues, fluid-filled cysts and tumors look different on this picture.
- Computed Tomography (CT) Scan - This is a method of body imaging in which a thin X-ray beam rotates around the patient. Small detectors measure the amount of X-rays that make it through the patient or particular area of interest. A computer analyzes the data to construct a cross-sectional image. These images can be stored, viewed on a monitor or printed on film. In addition, stacking the individual images or "slices" can create three-dimensional models of organs.
- Chest X-Ray - This X-ray provides pictures of the organs and structures inside the chest, including the heart and lungs an d the airway leading to them, major blood vessels, and upper portion of the thin sheet of muscle just below the lungs.
- Magnetic Resonance Imagining (MRI) - This is a painless non-invasive procedure that uses powerful magnets and radio waves to construct pictures of the body. Any imaging plane, or "slice" can be projected, stored in a computer, or printed on film. MRI can easily be performed through clothing and bones.
- Biopsy - This test involves removing a small piece of tissue for microscopic examination and/or culture, often to help your doctor make a diagnosis.
Treatment
When diagnosed and treated early, vulvar cancer can be cured in over 90 percent of cases. Treatment for vulvar cancer typically involves surgery, radiation therapy and in some cases, chemotherapy. Our team of cancer specialists, radiation specialists and plastic surgeons work together to design the most effective treatment plan for your condition.- Surgery - In many cases, vulvar cancer is treated with surgery. The type of surgery depends on the size, depth and spread of the cancer. One commonly used form of surgery is called wide local excision, in which the cancer and some of the normal tissue around the cancer is removed. Another surgical approach is called a radical excision, which removes the cancer and a larger portion of surrounding tissue and in some cases, the lymph nodes. After these procedures, patients may need to have skin from another part of the body added, or grafted, and plastic surgery to make an artificial vulva or vagina. In addition, in some cases, laser surgery may be used, which uses a narrow beam of light to remove cancer cells.
- Radiation Therapy - Radiation therapy uses X-rays or other high-energy rays to kill cancer cells and shrink tumors. Radiation may come from a machine outside the body, called external beam radiation therapy. Another form or radiation therapy, called internal radiation, works by placing materials that produce radiation, called radioisotopes, through thin plastic tubes into the area where the cancer cells are found. Radiation may be used alone, before or after surgery.
- Chemotherapy - Chemotherapy uses drugs to kill cancer cells. Drugs may be given by mouth, or they may be put into the body by a needle in the vein or muscle. Chemotherapy is called systemic treatment because the drug enters the blood stream, travels through the body, and can kill cancer cells throughout the body.
For more information, medical assessment and medical quote
as email attachment to
Email : - info@wecareindia.com
Contact Center Tel. (+91) 9029304141 (10 am. To 8 pm. IST)
(Only for international patients seeking treatment in India)










